IWC Educational Webinars & Training
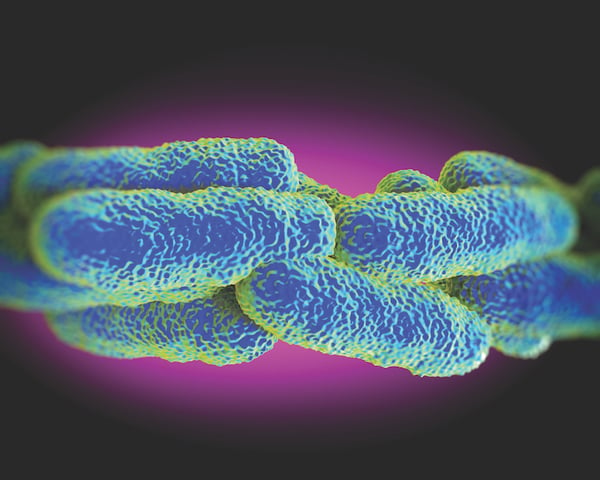
What is Legionella?
4 min read
IWC Innovations May 6, 2020

While water systems may not seem to be high on the priority list during the COVID-19 pandemic it is important for the health and safety of staff, patients and visitors that water systems are managed safely. Evidence from China (Zhou et al., 2020) is that half of COVID-19 fatalities had experienced a secondary infection. This suggests patients are at increased risk of secondary infections both during recovery and for some months after.
In the US and Europe just under 10% of community acquired cases of Legionnaires’ disease (pneumonia) prove fatal. If acquired in healthcare settings, the death rate can rise to >25%. The potential risks for Legionnaires’ disease and other waterborne infections may well be overlooked when planning for a rapid increase in the number of patients during the COVID-19 pandemic. This includes those suffering from COVID-19 and those transferred out of hospitals to make room for COVID-19 patients. They may have both an increased susceptibility to co-infection with other pathogens, including Legionella, during the pandemic as well as during the recovery and the gradual return to normal activities.
It is important to remember that water delivered to building and facility water system outlets is not sterile, even when complying with drinking water standards such as the SDWA (Safe Drinking Water Act) in the US. In systems which are not well designed or managed, microorganisms which are naturally occurring in water, including Legionella and Pseudomonas aeruginosa, can grow, colonize in biofilm and increase to levels which can cause severe illness and even death in very susceptible patients and staff. Legionnaires’ disease results when susceptible individuals become infected after inhaling fine mist or aerosols of water containing Legionella bacteria into their lungs from such simple water system devices as sink faucets and showerheads. This also includes any associated water systems or devices such as equipment used for ventilation and humidification. Aspiration is another potential mode of infection especially in those patients with swallowing difficulties, nasogastric feeding tubes or when sucking ice.
What sort of buildings is this guidance aimed for?
This guidance is aimed at healthcare facilities, care homes, nursing homes and other residential settings where there are patients and residents being treated for COVID-19 or for patients with increased susceptibility to infections such as those transferred from hospitals to make way for COVID-19 patients. The ongoing COVID-19 pandemic has a significant potential to increase the risks of waterborne infections, including Legionnaires’ disease. It is essential that appropriate testing of water systems and patients is carried out to protect both patients and staff from unrecognized outbreaks of waterborne infections including those caused by Legionella.
Where should I start?
Establish or consult with the multidisciplinary water management program Team or other person(s) responsible for water safety within the organization, using external expertise where needed. This should be done before plans are put in place to make changes to the water system such as adding temporary wards, wash hand basins, showers etc. and / or where additional equipment needs to be installed. Water systems and associated equipment should have up to date risk assessments and water management plans for controlling risks from Legionella. Where risk assessments and management plans are not up to date, or where there are any planned alterations or installation of additional equipment, the risk assessments and proposed water management plans should be appropriately reviewed. Advice should be sought from appropriate competent and experienced external consultants where required.
Factors which increase the risk of waterborne infections in staff and highly susceptible patients as a result of the COVID-19 response include:

Special requirements for water quality standards
Where there are special water quality standards required such as for dialysis, water used for humidification, ventilators, oxygen delivery etc., expertise should be sought from the relevant specialist suppliers. You should develop, and or modify, the water management plan (this can be by annotating the existing WMP by hand or adding an addendum) and ensure all actions are agreed by the team. Document how you will protect patients, staff, visitors and others from the presence of waterborne pathogens including Legionella. If required, get help from an experienced and competent water treatment advisor, public health or environmental health authorities.
Where local, state or national guidelines or legislation is in place then you must follow these.
Key points to remember
It is important to remember that Legionella and other waterborne pathogens of relevance in healthcare settings will grow in water systems to levels which may cause infection:
Let IWC Innovations Help Keep Your Building Safe From Legionella & other Waterborne Disease.
ESGLI - https://www.pwtag.org/esgli-guidance-managing-legionella-building-water-systems-covid-19-pandemic/

At a time when Legionnaires’ Disease outbreaks throughout the United States have increased fivefold, more people are being sickened by the Legionella...

How Does Legionella Grow Within the Water System?